#StudentMidwife recounts her experience at Sanctum Birth Center
Midwifery is an ancient profession; however, with the advancement of obstetrics, midwives have been marginalized all over the world. In the United States, midwives once trained through apprenticeship and practiced within their own communities. With the rapid growth of the field of obstetrics and movement of birth into hospitals during the 20th century, professional midwives in the U.S. today only attend ~10% of births, even while they are considered to be advanced primary health care providers on par with Advanced Nurse Practitioners.
In India, the traditional midwife or dai attended births in people’s homes. Today, the largest group of midwives are community health workers known as anganwadi or ASHA workers who undertake the gargantuan task of providing primary, antenatal, postpartum and pediatric care in rural areas. While there are options for nurses to train to attend births under OBGYNs, there is no option for professional training in midwifery. As a result, there are only a handful of Indian midwives who are able to practice independently in India. Two of them who are both U.S. trained CPMs (Certified Professional Midwives) have opened impressive birth centers — the Birth Village in Kochi, Kerala, and the Sanctum Birth Center in Hyderabad, Telangana.
The Sanctum Birth Center
I first visited the Sanctum Birth Center in 2018 and met Vijaya Krishnan, the midwife and owner. She had a doctorate in physical therapy prior to training as a midwife. I spent a month teaching prenatal yoga classes at Sanctum. When I started my own midwifery training, Sanctum was at the top of my clinical training list. Vijaya ma’am was gracious in accepting me as a student and extremely patient in navigating all the paperwork that was involved in getting my placement finalized, given that I was pursuing my midwifery degree through a U.S.-based institution.
The Sanctum Birth Center is categorized as a hospital, as Indian regulations for birth centers do not exist. It is located in a commercial complex, sharing a building with a supermarket and a night club! The center has six birthing rooms with birthing tubs, a double bed with an extra cot, bedside tables, a closet for storage and for necessary medications and supplies, an armchair, a chair without armrests, several stools of different heights, birthing balls, rebozos and an adjoining bathroom with a shower. There are appointment rooms, an operating theater, storage for IV stands, a sterilization area, oxygen tanks and nitrous oxide. The hospital is a Level 1 NICU facility and can do phototherapy as well. Newborn babies are only transferred to the nearby full-scope NICU if they need 24/7 observation or one-on-one pediatric care.

The center is owned and led by midwife Vijaya Krishnan who, in turn, has hired four affiliated OBGYNs who offer first-trimester care, back-up labor and birth care, perform C-sections when needed and consult on more complicated medical conditions that require collaborative care. An affiliated pediatrician offers pediatric care and is on call to assess newborns after each birth. An anesthesiologist is available on call to perform spinals or epidurals when necessary. The center is staffed 24/7 by nurses who work in pairs in shifts ranging from 6 to 12 hours.
As C-section rates have increased in India, clients who come to the birth center come specifically looking for a natural birth, with many seeking a water birth as well. In clinical circles, the term “natural birth” has largely fallen out of use and has been replaced with physiological birth. This change in nomenclature has taken place in order to validate all types of birth and not label surgery or other interventions as “unnatural”; however, even as language changes, clients continue to express their desires for a “natural” or “normal” birth, by which they largely mean a vaginal birth without interventions.
Antenatal Care
All clients are required to attend prenatal yoga, walk at least 40 minutes a day, eat a nutritious healthy diet and attend childbirth education classes (at which families are welcome!). As a result, hopefully, by the time their labor comes, they are physically and mentally prepared for birth, and solid partner and family support in place.
Diabetes and gestational diabetes are prevalent in the Indian population. In the U.S., I have seen GDM managed via standard protocols of testing using the one-step method; recommendations for diet, exercise and possibly medications; and finally induction at 38 weeks. I suspect it is managed similarly in hospitals in India as well; however, in the birth center, care is individualized.
In some cases, diabetes may present in the first trimester with an elevated A1c, while in others, GDM is noticed around 26 to 28 weeks with a 2-hour OGTT. Those with controlled diabetes and no other health complications may be accepted as clients, while those with uncontrolled values have higher risks, may not be good candidates for a birth center and are thus referred to a hospital. The birth center also takes care to classify people who are borderline GDM for whom only one value from their OGTT may have been slightly elevated.
First, lifestyle changes are recommended with a low-carbohydrate, high-protein diet personalized depending on each person’s 3-day diet diary, along with recommendations for walking after each meal for 30 minutes and practicing daily yoga. Follow-up fasting and postprandial values are drawn two weeks later, accompanied by regular check-ins to see if the diet and exercise routines are actually being followed. Almost always, if followed consistently, blood sugar values come down and are well controlled. If the values continue to be well controlled, often induction is not recommended until 41 weeks as long as macrosomia and poly/oligohydramnios are not of concern.
While those with hypertension are referred to hospital care, clients who have elevated hemoglobin in the second trimester, or those who have high-resistance umbilical arterial blood flow in their doppler and might be at risk for gestational hypertension are given a course of baby aspirin and their blood pressures are monitored closely. If gestational hypertension does occur, collaborative care with the OBGYN is started and medications are proscribed until induction is appropriate. In the few cases of gestational hypertension I saw during my time at Sanctum, all had vaginal births following the induction protocol.
The combination of a higher-than-average BMI and lower levels of physican activity meant that many clients have weak abdominal muscles that led to posterior positions or ROA/T positions, identified through leopold’s maneuvers. If at 36 weeks, and especially after 38 weeks, spinning babies positions (for example, side-lying hip release, forward-leaning inversion and cat/cow) are strongly encouraged and demonstrated within the antenatal visit.
People coming to the center from other parts of India have an initial virtual appointment and follow-up with local care providers where they reside before arriving in Hyderabad at 35 to 36 weeks. Most families rent a service apartment and stay until two weeks postpartum. I met people coming from as far away as Dubai, Singapore, Assam, Nasik, Chennai and Bangalore. There is also no obvious “type” of person who seeks care at Sanctum. The clientele are extremely diverse and hail from a range of different places, belong to multiple ethnicities and religions and are from a wide range of socio-economic classes.

Pain Relief
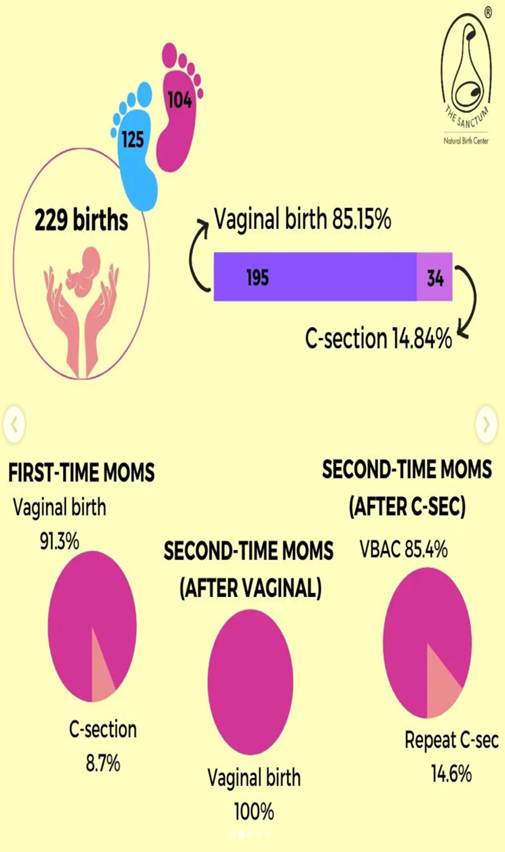
Everyone who comes to the birth center is advised that the facility only offers epidurals in case surgery is required, and it is extremely rare for an epidural to be employed for pain management during labor at the center. In fact, the rooms do not have the option for an epidural to be placed; one can only be placed in the operating room theater. As a result, people who come to birth at the center do not keep the option of an epidural in their mind as a backup method for pain relief. Pain relief is available from sterile water injections, hydrotherapy (bath or shower), hot water packs, birth ball, breathing and relaxation techniques, massage and comfort touch and one-on-one labor support and encouragement.

Labor
While at Sanctum, I witnessed several vaginal births which would almost certainly have resulted in Cesarean sections in most other birthing contexts. In particular, these were labors that stalled or took a long time to progress. This could happen in pre-labor or early labor at 2cm, between 5 cm to 7cm or even during pushing. Often the underlying cause was malposition, although occasionally it could be owing to a larger-sized baby.
Cervical checks are very minimally administered; however, when performed, more information than just dilation / station / effacement is gathered. Occasionally, a cervix swells and starts to close to one side; other times, it may continue to remain posterior; there may be an anterior or posterior lip; or it might be a baby with an asynclitic or posterior position.
Almost always, maternal positioning techniques are employed. These include doing the side-lying hip release for three contractions on each side, the forward leaning inversion for three contractions, five rounds of pancake flips (exaggerated side lying on each side, cat/cow, open knee chest), abdominal lift and tuck, walking, side lunges with the birth ball, rebozo sifting and full squats or time on the toilet seat. Often, this takes a couple of hours and is done by the nurses or the midwife. The commitment to positioning is extremely rigorous with the type of intensity you would see in a CrossFit class! The difference these interventions can make is often startling, with some people going from 6 cm to 9 cm within half an hour, or from 6 cm to head out in 3 hours.
When it seems like cervical dilation is not progressing as it should even with good contractions, a 2 ml IV dose of Drotin (Drotaverine Hydrochloride) is administered during a contraction to help speed up labors. Drotaverine Hydrochloride is not approved by the FDA; however, it has very few side effects. The evidence on it is of low quality, however, there is a suggestion that it could help shorten the length of labor, and further studies are needed. It is an antispasmodic medication that works on smooth muscle tissue, and therefore has an effect on the cervix. It may be repeated every half hour. We had a particular case where the birthing person had SROM at 38 weeks with light meconium. Once contractions began (within 24 hours) she progressed to 2.5cm, but then stalled for another 24 hours. At about 28 hours she was 6cm, but when the FHR had a few bradycardic episodes, Drotin was administered and the side lying hip release was done on both sides. She quickly progressed to 9.5cm within a half hour and was able to push the baby out in another hour.
Induction
Inductions at Sanctum are approached very cautiously. First, there is a lot of patience in recognizing when birth needs to be imminent as opposed to opting for expectant management (patiently waiting for labor to take its course). As mentioned before, if all is well, clients are counseled to wait for labor until 42 weeks.
Another significant difference is the manner in which inductions are managed. All clients are counseled at the first visit that in most cases, it is safe to wait until 42 weeks for labor to start. If an induction becomes necessary, but not urgent (as might be the case for gestational diabetes or ruptured membranes), natural induction methods are employed first.
The protocol to naturally induce labor involves an entire day of intermittent nipple stimulation and walking at the center. The birthing person arrives with their partner first thing in the morning and spends the entire day at the center, often until 9pm. They start with half an hour of nipple stimulation via breast pump (3 minutes on each side) followed by half an hour of walking and climbing stairs sideways (there are 7 floors in the building), and then a half hour of rest. Homeopathic medications are used; however, much like with the use of herbs, there is an art to the use of homeopathy. The most commonly used homeopathics are Belladonna, in difficult labors when the uterus or cervix remains rigid; Sepia, when the birthing person is tired from a difficult labor; Pulsatilla, to help transition from false labor to true labor; Gelsemium, for weakness and exhaustion or a long labor from a posterior presentation; and Rescue Remedy to combat exhaustion.
This protocol is repeated for 2 days, and most of the time labor starts on its own. Most often, contractions begin within 2 days, following which labor may progress on its own, or medical induction techniques (cervical gel if the cervix is still not softening and dilated, or synthetic oxytocin if dilation is about 3 to 4 cm) may be started if necessary.
If oxytocin is used, it is started at a very low dose (8 to 10 drops / min) and the fetal heart rate is checked every 15 minutes. Positional changes are continued even with augmentation, and all the pain relief techniques are employed as well. Synthetic oxytocin is rarely used when meconium is present or with those trying for a VBAC owing to the recognition that such medication might add additional stress to a fetus or uterus in more delicate situations.
Monitoring
Clients at Sanctum are recommended to get three ultrasound scans during pregnancy: the NT scan in the first trimester, the complete anatomy scan in the second trimester, and a growth scan at 36 weeks. Additional scans are only employed if there is a need for follow-up. Because scans can be unreliable, if an anomaly is present in the scan, there is thorough assessment to see if other parameters such as discrepancies in fundal height warrant further intervention.
At all antenatal visits and during labor, intermittent auscultation is employed. If necessary and appropriate, a 20-minute NST is completed anytime fetal wellbeing reassurance is needed. NSTs are conducted daily after rupture of membranes, if low fetal movement is reported, or after cervical softeners are inserted, but rarely used otherwise.
Water Births
There are a few criteria that are taken into consideration for people choosing to labor, or give birth in water. They should be low-risk; have a good FHR without any decels, intact membranes or membranes that have not been ruptured for more than 12 hours; and should not be at risk for PPH or shoulder dystocia. Unless water is being used in a prodromal early labor for relaxation, the contraction pattern has to be steady and strong enough to continue to progress when immersed.
The tub is filled enough so that the belly can be immersed and is around 100 degrees fahrenheit. Hydration is extremely important when in water, and intermittent auscultation with a doppler is continued. If any of the above conditions are not met, the midwife will ask the laboring person to exit the tub as any complication or concern that would make management more difficult in the water should be managed out of the tub. During the birth, the pelvis must be submerged in water. When the baby is born into the water, it is quickly placed skin to skin, and warmed with the towel. If there is no excessive bleeding, the placenta is birthed in the water as well! The sign of excess bleeding is if there is so much blood that you cannot see the bottom of the tub.
The water births are some of the most peaceful births that I have witnessed. People birthing in water appear to me more relaxed and often not just happy, but elated from the experience!
Breech
If a baby is in a breech position at 32 weeks, Spinning Babies techniques are taught and encouraged to be continued at home. This includes performing the side-lying hip release on both sides for 5 to 7 minutes followed by the forward leaning inversion and cat /cow a few times a day. If at 37 weeks, the baby still has not turned head down, an external cephalic version is attempted.
I witnessed a few ECV attempts, where first the Spinning Babies series was performed; then the pregnant person was cocooned in three rebozos and gently moved from side to side; and finally, the ECV was attempted slowly with fetal heart checks in-between and soft communication with the baby. Often if the baby is in a mood to kick and move, that can be a good sign for a successful version.
The first three ECVs that I witnessed were not successful, but for one client, it was repeated again at 39 weeks and succeeded then! This second-time parent went on to have a vaginal birth. For those whose ECVs are not successful, and who are good candidates, a vaginal breech birth is offered. I witnessed labor for a parent whose ECV was not successful and chose to attempt a breech birth. She was counseled on the risks and benefits and signed a breech birth release. Her labor began spontaneously around 39 weeks with spontaneous rupture of membranes. She then had contractions that got her to 6 cm, but then stalled for 10 to 12 hours. As augmentation wasn’t recommended, and while the FHR remained stable, a decision to perform a C-section was taken. The stalled labor was seen as a sign that either baby or body were not in a good place to continue to attempt a breech birth.
VBAC
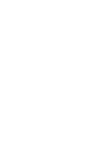
Telangana, the state in which Hyderabad is located, has the highest C-section rate in India. In private hospitals, the rate ranges from 60 to 90% (and from 30 to 40% in government hospitals). While many surgeries are by maternal request so as to schedule the birth for an “auspicious” time, skills and patience for physiologic and vaginal birth are also waning among practitioners. At the birth center, about one-third of the clientele are attempting a VBAC, and many travel from across the country so as to have that option.
When clients talk about their surgeries, their stories of unnecessary C-sections, lack of information or consent, and suffering verbal and physical abuse are extremely painful, and many are in tears as they recount their experiences. Just from charts, it is often clear that people were either bullied into inducing before their due dates or told their baby was “too large” or that it would be dangerous to wait even an hour after spontaneous rupture of membranes.
At the initial visit, after assessing whether a trial of labor after C-section might be appropriate, the risks and benefits are explained. Specifically, it is emphasized that while the center has an 85% success rate, there is a chance that a repeat surgery may be necessary. The biggest risk — that of uterine rupture — is explained, and the fact is shared that it may occur in 3 to 5 out of 1000 people trying for a VBAC. It is also explained that the only test for uterine rupture is a trial of labor, and that the signs of fetal heart rate changes, unusual bleeding or scar pain could be signs of separation.
The biggest challenge for VBAC clients is long labors from malpositioned babies due to weak abdominals. While diet, exercise and yoga are encouraged, all the same positioning techniques are employed to aid better positioning and faster labors. Since synthetic oxytocin is not used for VBAC clients, natural methods of induction are employed extensively. The only repeat C-sections that I witnessed were either due to extremely poor fetal movement followed by a concerning BPP on ultrasound, or due to adhesions from the previous surgery that did not allow the lower uterine segment to stretch as needed. Most successful VBACs were similar to primary physiological births, and some even had successful water births.
Episiotomy
Medio-lateral episiotomies are done when there is a need to get the baby out quickly or if the second stage has been extremely long and the baby is low enough. A few examples follow of what I have seen. In one case, an episiotomy was performed where the second stage was 6 hours, with no change for about 2 hours. Baby was at 0 station, caput at +2. While fetal heart tones were reassuring, the birthing person was absolutely exhausted from a long labor and pushing so an episiotomy was performed.
The second time I witnessed an episiotomy was in the case of a VBAC with a 5-day labor; while fetal heart tones were reassuring, she had GDM and was on insulin (her blood glucose was being tested regularly through labor to modify insulin as needed) and her levels spiked to 220 (even after insulin) when she had been pushing for 3 hours and baby was at +1. Because of the risk for hypoglycemia to the baby, an episiotomy was performed to help speed birth of the baby.
The third episiotomy I witnessed was for a birthing person who received an epidural after 12 hours of labor; the epidural was disconnected to help her push but during pushing the fetal heart tones were dropping to the 70s and so an episiotomy was performed to help birth the baby.
Consent is always obtained and lidocaine was used prior for all three episiotomies. Thankfully, all the babies did well after birth! So far no one has had an extended postpartum stay due to an episiotomy; however, the standard stay postpartum at this birth center is a night or two, which is longer than typically seen in birth centers in the U.S.
In case of emergencies
An OB is always either at the center or on call to be at the center as soon as required if necessary. Most of the time, they are called for a third or fourth degree tear and occasionally for surgery. An anesthesiologist is also available on call and comes in if surgery is necessary. The center’s pediatrician or the pediatric team from the nearby hospital is always present for the birth or to check the baby shortly thereafter.
Having an on-call system for providers means that early recognition of labor or fetal problems is imperative, even though OBs can generally be from call to incision within 30 minutes. Thankfully, as Vijaya ma’am says, “You don’t go from healthy to unhealthy in the blink of an eye. We typically have some time to react.” So if the fetal heart rate is not reassuring, thick meconium is present, or it seems like there is a chance for a shoulder dystocia from a larger baby, or if the birthing person has hypertension or gestational diabetes with symptoms during labor, the team is called early and kept ready just in case.
Postpartum
Most parents stay at the birth center for a day or two after birth. Nurses help with skin-to-skin and breastfeeding within the first hour, and continuously every couple hours as needed. Sometimes, the baby continues to breastfeed while suturing or surgical closure takes place. Vitals are monitored for the parent and baby, and visitors are welcome during the day. A pull-out cot is available in addition to the double bed.
For those who have had episiotomies or second-degree tears, infrared heat therapy is done to enable faster healing. The dry infrared heat stimulates blood flow, and, in particular, stimulates fibroblasts to aid in rebuilding collagen. The therapy is completed twice a day for three days with the birthing person sitting in front of the heat for about 10 minutes each time.
Parents are also encouraged to purchase a sitz bath, to immerse the perineum in warm water, and to apply Betadine a couple of times a day, as well as to avoid sitting cross-legged. The protocol seems to work well, as only those who failed to follow it had slower healing from what I witnessed.
Parents might return to the center for phototherapy within the first weeks if newborn jaundice is present or for breastfeeding support, while follow-up postpartum visits are at one week and six weeks postpartum; however, because the center has an integrated pediatrics practice, parents can also address any postpartum concerns at the one-month and other newborn visits.
Breastfeeding
In addition to continuous lactation support from the nurses, a lactation counselor visits all clients on day one post-birth. For low-risk people who do not have any colostrum within 48 hours after a physiological birth, Domperidone may be used to stimulate lactation. It is dosed at 10 mg three or four times per day, along with pumping to stimulate production every 3 hours. The baby is formula fed until milk is produced. The dose is kept for about 10 days after which it is slowly weaned off.
I have seen it used twice, both in parents who did not have any breast changes in pregnancy and where insufficient glandular tissue was suspected. In both cases, milk was produced within 48 to 72 hours of starting the medication, and combination feeding was done until the infant regained birth weight. If the infant continues to gain weight well, slowly the formula is weaned first, and then Domperidone is weaned. The infant then continues breastfeeding and pumped milk feeding until they are eventually able to exclusively breastfeed by 3 weeks or so. This approach took a village, a lot of support and immense dedication from the parents but was wonderful to see succeed!
Domperidone is not approved by the FDA in the U.S. due to risk of cardiac arrhythmias and QT prolongation. When it is used in India, it is only used in people without cardiac issues, and the risks of the medication, its side effects (dizziness, palpitations, syncope or seizures), and when to seek emergency care are clearly explained.
For babies that have a tongue or lip tie, parents are referred to a pediatric physician who specializes in releasing ties. Parents prep with a few days of exercises before the release, and follow up with the exercises after the procedure as well to maintain separation.

Conclusion
The Sanctum Birth Center is an excellent model of a midwifery-led birth center. It proves that midwifery care is extremely successful in creating good outcomes, with extremely high satisfaction for clients. If only we had more centers like this to universally offer midwifery and birth center care to everyone who desired such an option.
Neelu Shruti
Founder, Love Child Yoga