Frequently Asked Questions
FAQs and Answers
Is Gestational Diabetes an automatic reason for C-Section?
Gestational Diabetes (GD) is NOT an automatic reason for a C-Section. Using a combination of close monitoring, changes in activity level, exercise, diet it is possible for moms with GD to give birth naturally, in safe manner.
What is Gestational Diabetes (GD)?
The hormone Insulin plays critical role in Diabetes. The body needs glucose, a sugar, as a source of energy. Hormone Insulin helps glucose pass uniformly into the cells of the body where it is broken down into energy. Due to a variety of factors human body either stops production of Insulin or does not use Insulin in an efficient manner. This shows up as high glucose levels in the body and glucose passes out through urine. This can cause problems for the mother and for baby during pregnancy if she is diagnosed with Gestational Diabetes.
How do we diagnose GD?
At The Sanctum, we ensure that we gather as much information about mother’s health history, her family health history, her lifestyle, so that we can obtain a health profile of her. People whose family members (parents, grand parents etc) had diabetes are more susceptible to this condition. We make sure we have a very clear picture of mother’s health conditions and are proactive in putting together a care package for mothers who either have Gestational Diabetes or who may be candidates for Gestational Diabetes.
The most common test we use is blood tests to screen for Gestational Diabetes between 24th and 28th weeks of pregnancy. If we have prior knowledge of mother’s family health history or if we feel she may be highly prone to it, we may do the blood test earlier. If the tests come out positive for high glucose levels, we perform Glucose Tolerance Test (GTT) to confirm the diagnosis. This test requires that mother drink juice and subsequently blood is drawn every hour for a three-hour period.
Now that GD is confirmed how to treat it?
At The Sanctum, GD is more of controlling and management. We create a plan in consultation with the mother and her partner which balances her medication with changes in activity levels and Diet. This may involve Insulin shots if GD is higher than normal levels. The mother faces a higher chance of carrying her baby to full term if she is able to control her GD levels during pregnancy.
The most important controlling factors for GD are Activity and Diet. Exercise, Walking, Aerobics play a large role in burning up of those calories. We recommend our Prenatal Aerobics program for not only for women who have GD, but also for ALL to-be-mothers as it will help them burn calories during pregnancy, not only providing energy to them but also for their growing baby. If GD is not checked and controlled, baby receives increased levels of sugar which causes it to be at increased risk of having diabetes later on in life.
Wht is a typical Gestational Diet?
Perhaps even more important is a controlled Diet that allows the proper mix of proteins, carbohydrates and fat. Following is a sample Diet for Gestational Diabetes, especially for our Indian mothers:
- BREAKFAST
- Two Idlys, with 1 tbsp of coriander or pudina chutney OR
- Oatmeal with skim milk; 2 dates; 2 walnuts; 2 almonds; chopped apple or strawberry OR
- 1 or 2 eggs, boiled or as omlette
- MID MORNING
- Medium bowl of mixed fruit: Musambi, Apple or Orange OR
- 5-6 grapes OR
- 2 small cubes of paneer
- LUNCH
- 2 chapattis (jowar or multigrain atta) +
- small bowl of brown rice +
- 1 medium size cup of daal ( or chana or rajma or black eyed peas) OR
- 1 serving of non-veg or 1 egg + sabzi
- 1 cup of Dahi
- PLEASE INCLUDE either Palak, Methi, etc on a regular basis (as a source of Iron)
- ALTERNATE DIET FOR LUNCH
- Salad (also can be had as snack during the day)
- Lettuce, Spinach, Red Cabbage, Tomatoes, Cucumbers, Scallion (Green Onion), 2 cubes of paneer
- Dressing (make sure it does not have sweetener or high calories. Use Lemon, salt, 1/2 tsp of honey/vinegar with a touch of olive oil)
- Salad (also can be had as snack during the day)
- DINNER – Use similar conbination of LUNCH diet and alternate
One of the benefits of The Collaborative Model of Care at The Sanctum is that we apply the best aspects of the normal birth focused Midwifery Care in normal situations with selective aspects of Medical Management to bring Optimal, Safe and Satisfying birth for mothers who have conditions like GD. We are able to manage conditions like GD with inputs from our backup OB partner so that we give mothers the best of all worlds.
NOTE: While the above is a generalized Diet for Gestational Diabetes moms, please be very careful of using it on your own WITHOUT consulting your care provider. Each mother’s diet is carefully constructed based on detailed analysis of her condition and her family history. Every mother at The Sanctum receives a customized diet program based on HER specific situation, which may not be applicable or relevant to other moms.
In case you are interested in consulting with us and getting advice on correct Diet please fill out the Contact Us form or Call us at 72071 68666 and mention “Diet Counseling for Gestational Diabetes”. We will get back to you in 24-hours.
What is Cervical Insufficiency or Shortening
The Cervix
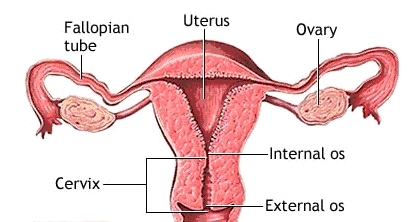
The cervix is the narrow, tubular, lower end of the uterus that extends into the vagina. When you’re not pregnant, the cervical canal remains open a tiny bit to allow sperm to enter the uterus and menstrual blood to flow out. Once you become pregnant, secretions fill the canal and form a protective barrier called the mucous plug. During a normal pregnancy, the cervix remains firm, long, and closed until late in the third trimester. At that point it usually starts to soften, shorten (efface) and open up (dilate) as your body prepares itself for labor.
Normally, in the late second and early third trimester the cervical length measures anywhere between 3 cm to 3.5 cm (30-35mm) and decreases progressively as the pregnancy advances, in preparation for labor (source: Obstetrics and Gynecology Board Review Manual).
The Problem
In cervical insufficiency, the cervix becomes softer and weaker than normal or is abnormally short to begin with. It may efface and dilate without contractions in the second or early third trimester as the weight of the growing baby puts increasing pressure on it. This condition can sometimes result in second term miscarriage, or premature rupture of the bag of waters, which can then result in preterm labor, especially before the 34th week.
Several studies have indicated that the likelihood of preterm delivery increases with decreasing cervical length. A cervical length of 25–30 mm before 32 weeks gestation seems to increase the risk of preterm delivery. If examination and ultrasound show that you have an abnormally short cervix, and you’re less than 24 weeks pregnant, your practitioner may recommend “cerclage”, a procedure in which she stitches a band of strong thread around your cervix to reinforce it and help hold it closed. However, there’s a lot of controversy about whether cerclage should be used in this situation.
Some recent research questions the effectiveness of the procedure at preventing miscarriage or preterm birth except in a small number of circumstances. And the procedure itself can lead to preterm delivery caused by uterine infection, ruptured membranes, and uterine “irritation” leading to contractions.
In certain other conditions, the benefits of cerclage can outweigh the risks. Women who seem to benefit from cerclage include those who’ve had three or more unexplained second-trimester losses or preterm births. If you’re in this group, you’re likely to get a cerclage at 13 to 16 weeks, before your cervix starts to change. A cerclage done then appears less risky than one done later in pregnancy, after your cervix has started to change. Once this procedure is done, you will be continually monitored by your obstetrician, until about 37 weeks, when the stitches can come out, and you can wait for labor to begin.
If this condition is discovered in the third trimester, bed rest or modified bed rest, would be the preferred choice, as opposed to cerclage. Although there’s no solid evidence that staying in bed is effective, the theory is that keeping the weight of the uterus off of a weakened cervix might help.
After going through a lot of recent research and literature, I have put together some recommendations for expectant mothers who are diagnosed with cervical shortening.
- Women with cervical measurements exceeding 26 mm should be just observed, and reassessed in 2-3 weeks.
- Women with cervical lengths between 21-25 mm should be placed on reduced physical activity, with re-measurement in 2 weeks.
- Women with cervical lengths between 16-20 mm should be placed on strict bed rest, with re-measurement in 1 week.Only women with cervical lengths of 15 mm or less should be considered for therapeutic cerclage.
- At this time, no evidence supports measuring cervical length or placing cerclage in the low-risk patient. This means, no scans and no other physical checks or interventions are recommended in the absence of symptoms and/or high risk in the expectant mother.
- While this is probably a good point of reference to start, it obviously needs to be taken within the context of the rest of your physical examination findings, and your obstetrician’s recommendations. In addition, your obstetrician will decide what the best intervention is for you, depending upon when your cervical shortening is diagnosed.
For more details on this particular topic you can look at information available in the following websites:
Cervical Insufficiency
Cervical Insufficiency and Short Cervix
At our practice at The Sanctum, we see quite a few women with Cervical Insufficiency and are able to closely manage their condition because of our unique Collaborative Model of Care. Our partner Ob/Gyn is very much involved in the care process to ensure the mother has the best of medical care also, in addition to the continuous, one-on-one care from our midwives. Our overwhelming natural birth rates for women with Cervical Insufficiency and even Cerclage in testimony to the success of our Collaborative Care Model of Care.
If you are facing a Cervical Insufficiency issue, or if you want a second opinion on your care provider’s decision to put a Cerclage do Contact Us for an appointment. In case you are outside Hyderabad we would be happy to counsel you via Skype.
The Power of Touch
One of the core principles of practice of the Midwifery Model of Care practiced at The Sanctum is Skin-to-Skin Contact between mother and baby as soon as the baby is born. Even after years of research scientists are only now beginning to uncover the proverbial “tip of the iceberg” as to the complex psycho-somatic messages that simple touch, accompanied by soothing voice of mother or father conveys to the newborn or the infant baby.
The act of touching your baby, caressing her, cooing softly to her creates protected space around her and you, that is only belongs to you and your baby, which for a moment is far removed from the humdrum of daily life and the stress accompanied with it. Research is showing that babies who are regularly caressed, touched lovingly by their parents tend to be calmer, sleep better and even show better brain development.
At our Natural Birth Center, The Sanctum every mother, without exception, has skin-to-skin contact with her baby as soon as she is born. Even in the rare case of a medically required c-section, as soon as the baby is brought out of the mother she is put on mother’s chest even while suturing is bring done. We see before our eyes the wonder of miracle that touch, eye contact between mother and her newborn and response of baby to her mother’s voice does to both.
Apart from the obvious electrifying emotion we have seen that the mother’s chest is probably the best Thermo-regulator for both her and her baby. And wonderfully, both mother and baby need each other in that precise moment because of the stress that both have gone through. The mother, through the intense labor process experience variety of emotions, changes in physical nature of her body including temperature swings and others. While our team of midwives and doulas are on hand at every moment of her labor, we recognize that this is nature’s incredible way of helping the mother deal with the process of childbirth. At the same moment, the baby too is passing through a constricted space, finding its way though crevices and passages in the birth canal, helped by the contractions of the uterus muscle, it too experiences a range of physical stress because of the restrictive environment. And when finally the baby is born into the vast outside world, it experiences changes that are enormous. Therefore laying on the protective chest of her mother assures baby that it is all right – the new environment will be as safe and secure as the old one inside her mother’s womb. And how so? As the mother coos to her baby and has her on her chest, as the baby experiences a rise in temperature, the mother’s chest simultaneously experiences fall in temperature. As bay’s temperature falls, mother’s temperature rises to keep the mother-baby unit stable. That is why we midwives consider MOTHER-BABY as a single unit. And the baby on her mother’s chest gets to listen to the same familiar heartbeat of her mother as she has been hearing from the time her sense of hearing started to function in the womb.
For the mother too, the act of caressing, touching her baby brings about lowering of stress as a result of increased production of Oxytocin, considered to be the “love hormone”. This hormone is recognized to be the single most important hormone throughout pregnancy, birth, and post partum. We have seen moms who have had very long, stressful labors immediately calm down and experience dramatic shift in mood the moment they have their baby on their chest and when they start to touch her and talk to her. And regular skin to skin contact with her baby, even for years after birth has been found to be positive for both mother and baby.
We recommend to all our parents to enroll in our Infant Massage Training as a means to connect with their babies in a way that is beneficial to both mother/father and the baby. Imagine a calm, quiet environment, with only you and your baby, eye-to-contact, soft whispering and cooing to your baby who responds back, you gently massaging your baby – it is guaranteed to bring a salubrious effect to you after a stressful day and a calming effect to your baby who will sleep with the memory of this wonderful moment with her mother or father. Infant massage is not only for moms – dads too can do it and it is our recommendation that they should too do it. After all, the baby has been listening to dads voices too while in the womb!


Midwifery Model vs Obstetric Model – a comparison

At The Sanctum, we have pioneered a unique Collaborative Model of Care – Women receive Independent Midwife Led Care, through pre-conception, pregnancy, labor, birth and postpartum, with back-up support and emergency infrastructure on site, in case of an emergency. Since 2009, our Birth Center has seen over 1000 births, with even higher risk women giving birth naturally, with routine VBACs, VBA2C, twin births and breech births. She believes strongly that respectful maternity care is the most important key to helping women have an informed and empowered birth. Our co-founder, Dr. Vijaya Krishnan and her team of midwives, using their gentle heart and hands, along with Evidence Based Midwifery Practices see the making of a strong confident mother who receives her baby with love and care. We believe that through education, advocacy and practice we can bring sustainable positive change in current birth practices in India, while using the Midwifery Model of Care.
Choosing who to be with you for your delivery should be a very personal decision. Yes, you will go by experiences of your friends and relatives but nothing cements your decision as a personal meeting between your potential care provider and you, your partner and your family. Midwives specialize in personalized, one-to-one interaction and have a family-centric care philosophy. So not only will they welcome your husband/partner in every checkup, she will also welcome involvement of your family. At The Sanctum, we have had parents, in-laws, sisters, aunts etc accompany mothers during their checkups. As long as it does not cause impediments in the care process we always welcome family involvement. After all, Midwifery Model of Care empowers women to be a significant part of the decision making process in how she wants to give birth.
Continuity of Care is a specialty of Midwifery Model. That means the midwife or the small team of midwives who takes care of you during your checkups will be the same person who will be with you during the birth. Midwives believe that apart from the physical care they provide, it is also in the ambit of care to provide you with emotional, psychological and social support. That means over the course of your pregnancy and during each antenatal checkup they will understand what your fears are, your preferences, your likes and dislikes and underlying reactions to certain situations. This helps them to proactively support you during the intense times of labor – many mothers feel and act in ways which they would not do under normal circumstances. A midwife, because she “knows” your personality will not be fazed by this and will understand why you are reacting the way you do, and will take care of the situation in the appropriate manner. In conventional hospitals because the OB/GYN has not taken the time or effort to get to know you so deeply will only react in the standard manner, either to medicate you to suppress your reaction, or if in extreme situations, wheel you to the operating table.
Midwives support new mothers after the birth, and will make sure you are able to breastfeed your baby and are able to care for her during the initial days. Because it is drastic and often overwhelming change for first-time mothers, midwives are your pillar of support, teaching you breastfeeding, guiding you through gentle exercises, tips on how to ward away post partum depression, or even act as counselors to you and your husband on how be partners in this new journey. Further, your midwife will help you through decision making on family planning, normal gynecological issues, etc. The same midwife is your friend, care provider and counselor through your entire pregnancy, new motherhood and beyond. At The Sanctum, the deep bonds of relationship with each of our mothers has still endured through many years, some as long as 10 years.
If you are pregnant, or looking to start a family, and want to evaluate the option of safe, natural, empowering birth, do give us a call at 72071 68666 and ask for an Initial Appointment. We would be happy to talk to you about your wishes and help you in your pregnancy, childbirth and post delivery care.


Talk to Us
Tips to follow to boost your chances of being pregnant
So how to increase your chances of conceiving and nurturing your pregnancy in a healthy manner? Download this e-bo0k which presents Tips to follow in order to boost your chances of pregnancy. We hope you find it useful. Please send us your feedback on how relevant you found the e-book to be.